Il piede torto è una deformità presente già alla nascita con alterazione dei rapporti tra le ossa del piede oltre che delle strutture capsulari, legamentose, muscolo-tendinee e fasciali. Esistono deformità differenti e gradi diversi di deformità, ciascuna delle quali prevede una terapia differente. L’osteopatia si può affiancare alla terapia medica (conservativa con apparecchi gessati o chirurgica), migliorando lo stato tensivo dei tessuti molli e aiutando quindi la correzione dell’atteggiamento viziato del piede. L’intervento osteopatico può anche alleviare il dolore post operatorio con il lavoro sulle strutture trazionate dalla cicatrice e permettendo un migliore adattamento delle varie strutture coinvolte. La prognosi è tanto più favorevole quanto più precoce è il trattamento sia medico, che osteopatico.
Tutti gli articoli di chiara
The effect of osteopathic treatment on the quality of life for male patients with urinary incontinence and Parkinson’s Disease
Di Francesco Badi
Abstract
Urinary incontinence caused by Detrusor Overactivity is a common problem between men suffering from Parkinson’s disease caused by the neurological degeneration of the dopaminergic neurones and this kind of symptoms could have an effect on Quality of Life of these patients. In particular nocturia and urinary urgency are the most annoying symptoms complained by patients. The aim of the present study was to evaluate whether osteopathic treatment could improve the urinary symptoms severity and have an effect on the Quality of Life.
MATERIALS AND METHODS: From 40 potential patient, 10 have been enrolled in the protocol, divided in two groups and the OAB-questionnaire was submitted to see changes before and after treatments. The patient of the Group 1 was treated before with 3 real osteopathic treatments and after with 3 “sham” treatments. The patient of the Group 2 did the opposite. OAB-q data were statistical analysed and compared.
STATISTICAL ANALYSIS: ANOVA: Data were analysed comparing data before treatments, after real osteopathic treatments, after sham treatments. ANOVA analysis of variance were used to analyse the variables that passed normality test except for “social” that was analysed with a Kruskal Wallis test. P was set at <0.05.
RESULTS: The results show no statistical significance for any variable but analysing the trend of the means of the single variable there are changes in every variable except for “sleep”.
CONCLUSION: Osteopathy seems not to be helpful in improving the quality of life of patient with incontinence suffering from Parkinson’s disease but it is worth to propose a larger study with a bigger sample of patient to clear these results.
INTRODUCTION
Parkinson’s disease (PD) is a neurological degenerative affection caused by the progressive loss of the dopaminergic neurones of the pars compacta in the substantia nigra of the basal ganglia. It affects 13.4 per 100,000 of the population (1). The typical clinical findings in these patients are: tremor, rigidity and bradikynesia (2). In addition to these symptoms there are also other non-motor symptoms in which there are depression, anxiety, sleep disorders, cognitive disorders (3) and autonomic disorders that can cause bladder dysfunction and urinary incontinence. The incidence of Lower Urinary Tract (LUT) disease has been estimated between 55% and 80% of PD patients (4). In Parkinson’s patients the thought is that the neural degeneration is not limited to basal ganglia but it involves other neural transmission systems outside the brain and the spinal cord (2). The voiding function is controlled by the pontine micturition centre (PMC) and it has been shown that it is facilitated by the hypothalamus, cerebellum, basal ganglia and frontal cortex (5). Studies suggest that bladder voiding is under the inhibitory control of the basal ganglia (5,6,7). These ganglia can control the dopaminergic neurons in the striatus nucleus which is responsible for the inhibition of the micturition reflex with a GABA-ergic circuit (8).
Sometimes the clinical findings about incontinence are not so clear because, in addition to a neurological problem due to the PD, other obstructive syndromes such as bladder outlet obstruction can be reported and this makes the diagnosis more complex (9). It has been found correlation between bladder dysfunction and neurological disorders in patients suffering from Parkinson’s disease (10) and between bladder dysfunction and stage of the disease (11). Another study by Campos-Sousa et al. did not find a correlation between the neurological degeneration and LUT symptoms (12). Of the symptoms complained of nocturia is the most common among Parkinon’s patients (>60%) (10,11,12). Detrusor overactivity has been found in 45-93% (13) and a relaxation of the external sphincter in 33% of the cases (14).
In literature there are no articles about manual treatments in this kind of patient but there are some authors that underline the importance of the treatment of the pubo-prostatic ligaments to improve the continence in overactive bladder (15,16). Studies mention some parts of the body that if treated may help to balance the autonomic nervous system and reduce stress on the walls of the bladder so as to improve the continence(17).
Study Aims
The aim of this study was to investigate whether osteopathic treatment has an effect on:
1. Urinary incontinence in men suffering of PD
2. The Quality of Life of men suffering of PD.
The hypothesis was that the treatment of the Dorsal-Lumbar spine, which is the tract of the sympathetic innervation of the LUT, and the treatment of the pelvic floor and thoracic diaphragm, to balance the intra-abdominal pressure, could improve the voiding symptoms in these patients and affect their Quality of Life.
METHODOLOGY
Participants
Participants were men recruited from the degenerative illness division of the Valduce Hospital in Como, Italy who were invited to participate in the study. From 40 men between 50 to 70 years old identified as potential patients, 10 men decided to join the study. To enter the study they must have suffered from Parkinson’s Disease for over 5 years and from urinary incontinence for over 2 years. Patients who have had tumours or surgical intervention on the bladder were excluded from the study, also excluded was a patient who had a LUT infection during the clinical trial. Patients also suffering from other disease e.g. Diabetes Mellitus were excluded. (Table 1)
| INCLUSION | EXCLUSION | |
| AGE | 50-70 years old | <50years >70years |
| PARKINSON | >5 years | <5 years |
| INCONTINENCE | >2 years | <2 years |
| SURGICAL INTERVENTION ON BLADDER | No | Yes |
| LUT INFECTION | No | Yes |
| OTHER DISEASE | No | Yes |
Table 1: Inclusion/Exclusion criteria.
Materials & Methods
Men were selected among the degenerative illness division of the Valduce hospital and evaluated by Dr Corengia who assessed the risk and benefits of the osteopathic treatment and who determined whether the patients were appropriate to be included in the study.
An information sheet about the study explaining the aims, the procedure, the single treatment (Appendix I) and Risk Assessment Sheets (Appendix II) was given to the subjects. Participants were also required to sign a consent form after joining the study (Appendix III). The validated Overactive Bladder Questionnaire (18,19) was given to participants to assess the initial urinary symptoms and Quality of Life rating and to monitoring the improvements with OMT before and after treatments (3,20) (Appendix IV).
Experimental Procedure
The 10 patients who were recruited to take part to the study were randomly divided in two groups:
Group 1_ Subjects were treated with OMT for three times and after with a sham treatment for another three times with a wash out period of two weeks between OMT and sham
Group 2_ Subjects were treated with sham treatment before for three times, and after with OMT for another three times with a wash out period of two weeks between sham and OMT.
Osteopathic Treatment: Subjects were treated with mobilization of the dorsal-lumbar spine because of the sympathetic innervation of the LUT trying to balance the sympathetic autonomic system, and had the thoracic diaphragm and pelvic diaphragm assessed because of the intra-abdominal pressure that can cause incontinence. Patients had their pubic symphysis and the pubo-prostatic ligament of the urogenital diaphragm assessed with palpation because the fascial treatment of these ligaments improve the bladder continence (15,16,17).
Sham treatment: Subjects were treated at a different part of the body so as not to interfere with the intervention treatment. The sham treatment was designed to appear as a valid treatment to the subjects.
Subjects were sham treated on the Lower Limb so as not to interfere with the interventional treatment. The sham treatment had interventional parameters equal to the treatment but on the “neutral “ area.
Apparatus
The OAB-questionnaire was given to participants before any treatments started, after real osteopathic treatments and after the sham treatments. The Overactive Bladder Questionnaire (OAB-q) is a multidimensional instrument designed to assess patient perception of symptom complained and its impact on health-related quality of life (HRQL) among patients with Overactive Bladder. This questionnaire is composed of 33 items that involves the evaluation of the urinary symptoms severity and its affect on the Quality of Life in the first 8 items, and the other 25 items are a general investigation of the Quality of Life of the subjects through the evaluation of different aspects (concern, coping sleep, social interaction) (18).
Ethical Issues
The subjects were recruited by invitation to voluntarily take part in the study. All questionnaires were anonymous. The subjects retained the right to stop the procedure and leave the study at any point, without giving a reason. Their ongoing drug treatment was neither stopped nor changed during the research project. The ethic form was submitted and approved by BCOM (Appendix V).
STATISTICAL ANALYSIS
Data were analysed comparing data before treatments, after real osteopathic treatments, after sham treatments. A normality test was run (Shapiro Wilk) for this data. Every variable passed the normality test except for the “social” variable. ANOVA was used on the variables that passed normality, the “social” variable (that failed normality)was analysed with a Kruskal Wallis test. The means of the single variable were also analysed to see changes even without a statistical significance. P was set at <0.05.
RESULTS
All of the 10 patient complete the study no one quitted it. The mean age of the participants was 67.5 years old.
The results show no statistical significance with the ANOVA analysis. No differences has been found with the variable “group”.
“Symptoms Severity”, though the symptom results show a trend of improvement for both post OMT and post sham this did not reach statistical significance (F=0.529 p=0.595; Graph 1). Sleep showed no change over the three interventions (F=0.086; p=0.018; Graph 2)
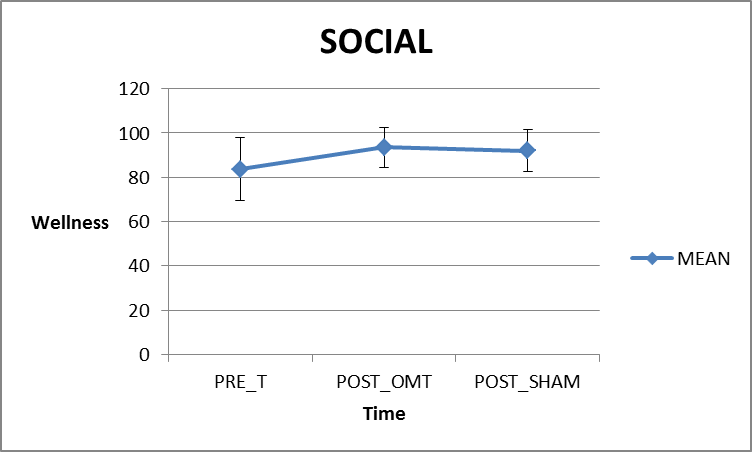
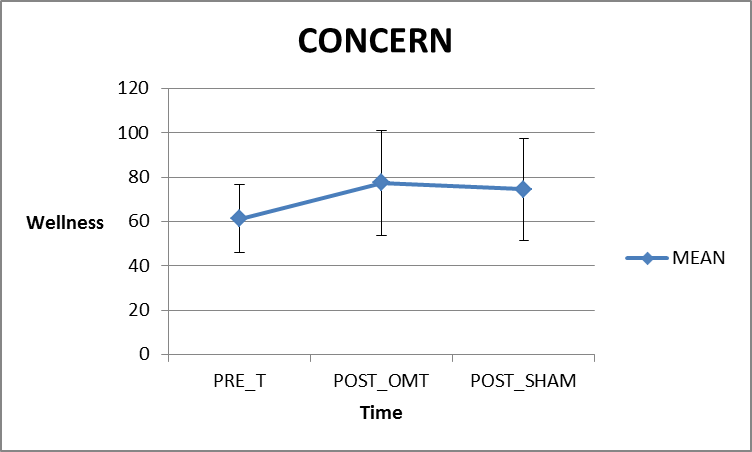
“Coping’ showed no significant difference between pre, post OMT or post Sham (F=0.421 p=0.661; Graph 4). ‘Social’ showed a slight improvement from the pre questionnaire but did not reach statistical significance (Kruskal Wallis test, H=3.614, p=0.164; Graph 3). ‘Concern’ though the symptom results show a trend of improvement for both post OMT and post sham this did not reach statistical significance (F=1.661, p=0.209; Graph 5).
 GRAPH 1: Symptom severity (0=no symptoms). Graph showing the mean values of the Overactive Bladder Questionnaire. Error bars= SD and n=10. There was no statistical significance for any group. There is a slight improvement from pre-treatments and after OMT treatments but after the sham treatments there is a little worsening. A global improvement from before treatments and after treatments.
GRAPH 1: Symptom severity (0=no symptoms). Graph showing the mean values of the Overactive Bladder Questionnaire. Error bars= SD and n=10. There was no statistical significance for any group. There is a slight improvement from pre-treatments and after OMT treatments but after the sham treatments there is a little worsening. A global improvement from before treatments and after treatments.
GRAPH 2: Sleep (100 =complete wellbeing ). Graph showing the mean values of the Overactive Bladder Questionnaire. Error bars= SD and n=10. There was no statistical significance for any group. There is no substantial changes between before and after treatments.
GRAPH 3: Social (100 =complete wellbeing ). Graph showing the mean values of the Overactive Bladder Questionnaire. Error bars= SD and n=10. There was no statistical significance for any group. There is a slight improvement between pre- treatments and after OMT treatments and a little worsening after the sham treatments. A global improvement from the beginning of the therapy to the end.
GRAPH 4: Coping (100 =complete wellbeing ). Graph showing the mean values of the Overactive Bladder Questionnaire. Error bars= SD and n=10. There was no statistical significance for any group. There are no substantial changes between before treatments and after OMT, and a slight improvement after the sham treatments.
GRAPH 5: Concern (100=complete wellbeing ). Graph showing the mean values of the Overactive Bladder Questionnaire. Error bars= SD and n=10. There was no statistical significance for any group. There is an improvement from before treatments and after OMT treatments, and a little worsening after the sham treatments.
DISCUSSION
Urinary incontinence caused by neurogenic Detrusor Overactivity is a common finding in patients suffering from Parkinson’s disease, and its affect the quality of life, emotional well-being and productivity at work (21).
The OAB-questionnaire is a validated questionnaire to identify Overactive Bladder (OAB) that a symptom-based condition defined as “urinary urgency with or without incontinence, often with increased urinary frequency and nocturia” (18,19). Although the results from this current study did not reach a statistical significance, the means of the single variables suggest that there are a trends of improvements in the variables “symptoms severity” “social” and “concern” after OMT treatments and no substantial changes in the variable “sleep”, which did not have changes, and “coping” which has a slight improvement after the sham treatments. In a general overview of the means of the single variable which are not statistically significant, it can be noticed that between before and after all treatments there is an improvement in every variable except for “sleep”. In the current literature there are no other studies about manual treatments and Overactive Bladder. The small number of patients led to slight results in symptoms severity with no statistical significance, but the mean differences suggest that Osteopathic Manual Treatment could have an effect of these symptoms and on the Quality of Life of the patients.
Detrusor Overactivity is thought to be the most probable cause of Overactive Bladder (22) but there is also another condition that can cause similar urinary symptoms: the Bladder Outlet Obstruction (e.g. prostatic hypertrophy). The Bladder Outlet Obstruction is a common condition that can affect men over 50 years old and can be added to a clinical condition of Overactive Bladder (23). For these reasons it cannot be reported if the Osteopathic treatment had an effect during this intervention on autonomic nervous system balancing the sympathetic and parasympathetic system or intervention reducing mechanical stress over the bladder and Lower Urinary Tract. Furthermore the Bladder Outlet Obstruction can change the afferent nervous signal from the Lower Urinary Tract itself and cause an imbalance of the sympathetic/parasympathetic system (24).
The Quality of Life of these patients is heavily affected by the urological symptoms that can reduce the sleeping time, social interaction and increase the time spent at home (25).
It is well known that osteopathy can significantly affect the Quality of Life of patients with several pathologies (26,27) however this current study did not show any significant changes in the quality of like of these patients. This may be due to the limitations discussed later in this paper.
Limits of the study
The small sample of patients is a great limitation of the current study, the statistical tests showed that each variable was under powered (<0.8) and a sample size calculation suggested a minimum of 50 participants would be needed. The inclusion/exclusion criteria limited the size of the sample because women and men have anatomical differences and different types of incontinence caused by other reasons; for these reasons the sample was exclusively men (28). Furthermore we have no difference between pre-treatments and post-treatments statistically significant so we cannot consider these results as positive results. This could be due to the small sample of patient that is hard to find among Parkinson’s patient because is a problem underrated by doctors and the patients are not stimulate to complain about these symptoms because they feel embarrassed. It could have been used a more specific questionnaire on bladder symptoms perception in addition to OAB-q such as the PPBC (Patient Perception Bladder Condition) (29). The study would have been more specific with the help of objective measures for instance a cystometry or urodynamic exams to assess the initial level of the disease and the changes after treatments (30). The short time of recruitment may be considered as a limitation because patients with these characteristics are available only in particular clinics or hospitals and they have only a small number of patients.
CONCLUSION
The current study show that osteopathy cannot change aspects of the Quality of Life in patient suffering from incontinence and Parkinson’s disease. Some changes were recorded with the trend of the analysis of the means so further studies with a larger sample of patients are needed to clear these aspects.
References:
- Stephen K. Van Den Eeden, Caroline M. Tanner, Allan L. Bernstein, Robin D. Fross, Amethyst Leimpeter1 Daniel A. Bloch, and Lorene M. Nelson, Incidence of Parkinson’s Disease: Variation by Age, Gender, and Race/Ethnicity, American Journal of Epidemiology,2003 Vol. 157, No. 11.
- Sakakibara R, Tateno F, Kishi M, Tsuyuzaki Y, Uchiyama T, Yamamoto T., “Pathophysiology of bladder dysfunction in Parkinson’s disease.” Neurobiological Disease. 2012 Jun;46(3):565-71.
- Kristine K. Hanna and Alice Cronin-Golomb “Impact of Anxiety on Quality of Life in Parkinson’s Disease” Parkinson’s Disease 2012, Article ID 640707
- McGrother, C.W., Jagger, C., Clarke, M., Castleden, C.M., 1990. Handicaps associated with incontinence: implications for management. Journal of Epidemiology and Community Health 44,246–248.
- Kavia, R.B.C., Dasgupta, R., Fowler, C.J., 2005. Functional imaging and the central control of the bladder. Journal of Comparative Neurology 493, 27–32.
- De Groat, W.C., 2006. Integrative control of the lower urinary tract: preclinical perspective.British Journal of Pharmacology 147, S25–S40.
- Blackett H, Richard Walker, Brian Wood, “Urinary dysfunction in Parkinson’s disease: A review” Parkinsonism and Related Disorders 15 (2009) 81e87
- Dalmose, A.L., Bjarkam, C.R., Sorensen, J.C., Djurhuus, J.C., Jorgensen, T.M., 2004. Effects of high frequency deep brain stimulation on urine storage and voiding function in conscious minipigs. Neurourology and Urodynamics 23, 265–272.
- Gina A Defreitas, Gary E Lemack, Philippe E Zimmern, Richard B Dewey, Claus G Roehrborn, Padraig E O’Suilleabhain, “Distinguishing neurogenic from non-neurogenic detrusor overactivity: a urodynamic assessment of lower urinary tract symptoms in patients with and without Parkinson’s disease” Urology. 2003 Oct;62(4):651-5.
- Araki I, Kitahara M, Oida T, Kuno S. “Voiding dysfunction and Parkinson’s disease: urodynamic abnormalities and urinary symptoms”. Journal of Urology 2000 Nov;164(5):1640-3.
- Sakakibara, R., Shinotoh, H., Uchiyama, T., Sakuma, M., Kashiwado, M., Yoshiyama, M., Hattori, T., 2001. Questionnaire-based assessment of pelvic organ dysfunction in Parkinson’s disease. Autonomic Neuroscience:Basic&Clinical. 92, 76–85.
- Campos-Sousa, R.N., Quagliato, E., da Silva, B.B., De Jr., C.R., Ribeiro, S.C., de Carvalho, D.F., 2003. Urinary symptoms in Parkinson’s disease: prevalence and associated factors. Arquivos de Neuropsiquiatria 61, 359–363.
- Palleschi G, Pastore AL, Stocchi F, Bova G, Inghilleri M, Sigala S, Carbone A., “Correlation between the Overactive Bladder questionnaire (OAB-q) and urodynamic data of Parkinson disease patients affected by neurogenic detrusor overactivity during antimuscarinic treatment.” Clin Neuropharmacol. 2006 Jul-Aug;29(4):220-9.
- Hattori, T., Yasuda, K., Kita, K., Hirayama, K., 1992. Voiding dysfunction in Parkinson’s disease. Jpn. J. Psychiatry Neurol. 46, 181–186
- Raymond E PooreA, David L McCulloughA, Jonathan P JarowA, Puboprostatic Ligament Sparing Improves Urinary Continence After Radical Retropubic Prostatectomy,Urology, Volume 51, Issue 1, January 1998, Pages 67–72
- Siamak Daneshmand, David A. Ginsberg, James K. Bennet, Jenelle Foote, Wylly Killorin, Kevin P. Rozas, Bruce G. Green, Puboprostatic Sling Repair for Treatment of Urethral Incompetence in Adult Neurogenic incontinence, Journal of Urology, Volume 169, Issue 1, January 2003,
- Kuchera M. Kuchera W “Osteopathic consideration in systemic disfunction” Columbus Greyden Press 1994, Osteopathic consideration in genitourinary tract disorders;
- Coyne KS, Matza LS, Thompson CL. The responsiveness of the Overactive Bladder Questionnaire (OAB-q). Quality of Life Research 2005;14(3): 849Y855.
- Wein AJ. Diagnosis and treatment of the overactive bladder. Urology. 2003 Nov;62(5 Suppl 2):20-7.
- Karin S. Coyne, Chris C. Sexton, Debra E. Irwin*, Zoe S. Kopp†, Con J. Kelleher‡ and Ian Milsom The impact of overactive bladder, incontinence and other lower urinary tract symptoms on quality of life, work productivity, sexuality and emotional well-being in men and women: results from the EPIC study, BJU International Journal (2008)| 101 , 1 3 8 8 – 1 3 9 5
- Debra E Irwin, Ian Milsom, Zoe Kopp, Paul Abrams, Linda Cardozo, Impact of overactive bladder symptoms on employment, social interactions and emotional well-being in six European countries, BJU International volume 97, Issue 1, pages 96–100, January 2006
- Andersson KE. The overactive bladder: pharmacologic basis of drug treatment . Urology 1997 ; 50 ( 6A Suppl ): 74 – 84
- Ali A, Al-Zahrani AA, Gajewski JB. Association of symptoms with urodynamic findings in men with overactive bladder syndrome. BJU International 2012 Dec;110(11 Pt C):E891-5.
- Dobrek L, Baranowska A, Skowron B, Thor PJ. Autonomic nervous system activity assessement by heart rate variability in experimental bladder outlet obstruction Postepy Hig Med Dosw (Online). 2013 Apr 2;67(0):221-8.
- Espuña-Pons M, Castro-Díaz D, Díaz-Cuervo H, Pérez M. Impact of overactive bladder treatment on the quality of life of patients over 60 with associated pathologies Archivos Espanoles de Urologia. 2013 Apr;66(3):287-294.
- Florance BM, Frin G, Dainese R, Nébot-Vivinus MH, Marine Barjoan E, Marjoux S, Laurens JP, Payrouse JL, Hébuterne X, Piche T Osteopathy improves the severity of irritable bowel syndrome: a pilot randomized sham-controlled study, European Journal of Gastroenterology and Hepatology. 2012 Aug;24(8):944-9
- Papa L, Mandara A, Bottali M, Gulisano V, Orfei S. A randomized control trial on the effectiveness of osteopathic manipulative treatment in reducing pain and improving the quality of life in elderly patients affected by osteoporosis. Clin Cases Miner Bone Metab. 2012 Sep;9(3):179-83.
- Giarenis I, Mastoroudes H, Srikrishna S, Robinson D, Cardozo L. Is there a difference between women with or without detrusor overactivity complaining of symptoms of overactive bladder? BJU International 2013 Mar 4.
- Karin S. Coyne a, Louis S. Matzaa, Zoe Koppb, Paul Abrams, The Validation of the Patient Perception of Bladder Condition (PPBC): A Single-Item Global Measure for Patients with Overactive Bladder, European Urology 49 (2006) 1079–1086
- Simn Jackson, The patient with an overactive bladder—Symptoms and quality-of-life issues, Urology volume 50, Issue 6, Supplement 1, December 1997
Bachelor Science in Osteopathy
Il B.Sc. Ost (Bachelor Science in Osteopathy) è un titolo accademico riconosciuto a livello internazionale, al momento quello maggiormente conseguito in Europa per la pratica della professione osteopatica.
Tale titolo viene rilasciato, tra le altre università europee, da BCOM (British College of Osteopathic Medicine), una delle più prestigiose scuole di osteopatia del Regno Unito. La conversione del Diploma in Osteopatia, titolo rilasciato dalla scuola italiana, in Bachelor Science in Osteopathy, rilasciato dall’università londinese, è possibile grazie alla collaborazione tra AIMO e BCOM.
Il percorso di conversione prevede un’interazione con i docenti dell’università inglese che si conclude con la realizzazione di un progetto di ricerca, la stesura e l’esposizione in lingua inglese della tesi di laurea.
“Effectiveness of osteopathic treatment on infantile colic” di Chiara Frittoli
Diploma in Osteopatia
Il D.O. (Diploma in Osteopatia) è un titolo che viene rilasciato al termine di differenti percorsi di studio osteopatico. Gli osteopati di Ostmonza hanno scelto di garantire le proprie competenze ai pazienti optando per il corso full time presso realtà accademiche i cui professionisti rispettano gli standard indicati dai documenti internazionali FORE (Forum for Osteopathic Regulation in Europe), FEO (Federazione Europea degli Osteopati), OMS (Organizzazione Mondiale della Sanità).
Il corso di osteopatia full time si articola in 5 anni dei quali i primi 2 sono dedicati allo studio di materie teorico-scientifiche e ad un primo approccio manuale, che si sviluppa poi dal terzo anno nel tirocinio clinico dove si pratica su pazienti reali.
Al termine del corso di osteopatia full time vengono completate 3000 ore di lezioni teorico-pratiche e 1200 ore di tirocinio clinico.
Effectiveness of osteopathic treatment on infantile colic
INTRODUCTION
The aim of this current study was to assess if Osteopathic Manual Treatment (OMT) has an effect on babies’ colic, considering the change of all the variables of behaviour in a day (sleeping, awake & content, feeding, fussy, crying and unsoothable crying). Moreover not only cranial as in the UK pilot study, but an osteopathic treatment on the entire body was tested.
METHODOLOGY
Participants
The present study, a clinical trial, compared the effects of a phytotherapic product alone with the effect of phytotherapy combined with OMT. 10 participants were recruited through local paediatricians. Treatments were performed by the same osteopath. The research protocol was approved by the BCOM Ethics Committee (Appendix I).
To participate in the study, infants needed to fulfil certain inclusion criteria (Table 1) that feature the colic period [1] and be healthy babies [14]: aged between 2 weeks and 3 months of life, gestational age between 37 and 42 weeks, birth weight between 2.5 and 4 kg, an Apgar index more or equal to 7. Mothers and babies had to be healthy during pregnancy, birth and until the beginning of the study (a part from colic). No limits were put in relation to type of delivery, as others have shown it has no influence on colic trend [15]. Furthermore babies needed to be exclusively breastfed and mothers were requested not to alter their diet during the study period [16-18].
|
INCLUSION |
EXCLUSION |
|
|
AGE |
3 weeks-3 months |
<3 weeks >3 months |
|
GESTATIONAL AGE |
37-42 weeks |
Pre-terms and post-terms |
|
BIRTH WEIGHT |
2.5-4 kg |
<2.5 kg >4 kg |
|
APGAR |
≥7 |
<7 |
|
PREGNANCY |
Healthy |
Complicated or Pathological |
|
BIRTH |
Healthy |
Complicated or Pathological |
|
LIFE |
Healthy a part for colic |
Pathologies |
|
BABY’S FEEDING |
Exclusively breastfeeding |
Bottle or mixed feeding |
|
MOTHER’S FEEDING |
No changes in the diet during the study |
Change in the diet during the study |
|
TREATMENT |
No previous manual Treatment |
Previous manual treatment |
|
Table 1: inclusion and exclusion criteria |
||
Methods
Infants were selected from paediatricians and were diagnosed with colic by means of the Crying Pattern Questionnaire [19-20] (Appendix II).
A written basic explanation of aims, procedure and possible risks of the project were given to the parents/guardians by way of Information (Appendix III) and Risk Assessment Sheets (Appendix IV). Parents were required to consent to take part in the study, after reading these documents by signing the written Consent Form (Appendix V). The babies’ eligibility was confirmed by the Questionnaire (Appendix VI) completed by the parents/guardian about their babies medical history.
During the study the parents were asked to record in a validated Daily Diary [21-22] (Appendix VII) the baby’s behaviour in terms of hours/24 spent sleeping, crying, fussing, feeding and awaking. Details of how to record types of behaviour were explained in the Instruction Sheet (Appendix VIII).
Procedure and Ethical Issues
Babies recruited needed to cry at least 3 hours/day, as mean of the data recorded in the diary during the first 3 days of the study.
Because of the age of the babies some precautions were taken to protect them: a sham treatment was avoided and every infant received with no interruptions at least a treatment having the possibility to try both medical and osteopathic treatment. All data was kept anonymous in the study.
Infants initially attended the control group for 2 weeks, during which they were treated by a standard medical treatment (SMT); it consisted of a phytotherapic product used following the paediatrician’s instruction explained in the Standard Medical Treatment Sheet (Appendix IX). During the 2nd week of SMT, the parents completed the diary, from which babies who cried more than 3 hours per day (as mean of the data recorded) took part in the treatment group. The phase consisted of 3 treatments, a treatment each week for 3 weeks, that lasted about 30 minutes and consisted of gentle cranial and fascial techniques. During the OMT period, manual treatments remained coupled with SMT. During the 3rd week of OMT+SMT parents completed the diary.
Osteopathic Manual Treatment
Treatments were based on the concept of the black box: not a single technique or a standard treatment for every patient, but the approach of every single dysfunction found in the individual patient. In particular, the anatomic regions analysed were:
- JUGULAR FORAMEN: this foramen is the vagus nerve exit that carries to the brain the 95% of gastrointestinal tract afferent messages. Occipital or temporal dysfunctions can distort the jugular foramen, with possible consequences on vagal function [23]. Infants born through a natural delivery showed different cranic base dysfunctions [24].
- DORSO-LUMBAR SPINE: this is the metameric level of the bowel ortosympathetic innervation. Somatic dysfunctions at this level may interact with afferent and efferent signals improving the pain sensation, deteriorating the bowel activity [25].
- UPPER CERVICAL SPINE: vagus and trigeminal nerve are in communication through the spinal trigeminal nucleus. A recent study showed that repeated low intensity stimulus on the vagus nerve gives further stimulus to the trigeminal nucleus, inhibiting it [26]. Somatic dysfunctions of the first cervical vertebrae (where trigeminal nucleus is located) may interact with vagus afferent signals and lead to a distorted message to the vagal nucleus responsible of gastrointestinal tract innervation.
- DIAPHRAGM: one of the possible causes of colic is excess gas in the bowel, which may increase abdominal pressure [1]. Moreover the increased pressure may prevent gas ejection. Osteopathic research has shown that treating the diaphragm may modify intra-thoracic and intra-abdominal pressure [27]. The treatment covered also the other diaphragms (cranic and pelvic, superior thoracic aperture) with which the thoracic diaphragm should harmoniously work [28].
- DIGASTRIC AND SWALLOWING MUSCLES: a hypothesis about pain aetiology during baby’s feeding concerns the spasm of the swallowing muscles [29]. These muscles provoke pain only in the first weeks of life probably because later, getting stronger, the risk of spasm is reduced as in an athlete the muscle strengthening delay soreness onset [30]. The inhibition of digastric and supra-hyoid muscles or the correction of hyoid bone dysfunction may reduce this pain.
Statistical analysis
The endpoints of the study were the parameters recorded in the diary: the mean number of hours/24 in each week of the study spent in sleeping, awake & content, fussing, crying, unsoothable crying and feeding. For each infant the difference of the mean (table 2) of these parameters were valuated from time 0 (T0) to time 1 (T1), from T1 to time 2 (T2) and from T0 to T2. T0 was the time before the beginning of the study, during which babies received no treatments. T1 was the second week of the study, during which infants were treated with SMT, a week after the use of phytotherapic product. T2 was the fifth week of the study, during which babies were treated with OMT+SMT, after the third manipulative treatment. Then the mean difference was tested for significance with repeated measures one way ANOVA for each variable. When test for normality (Shapiro wilk) failed ANOVA on ranks was performed. The software used was SigmaPlot (version 11), post hoc analysis was performed through the Tukey test. P<0.05 was considered statistically significant.
|
SLEEPING |
AWAKE & CONTENT |
FEEDING |
FUSSY |
CRYING |
UNSOOTHABLE CRYING |
|
|
T0* |
10.56 |
4.58 |
3.44 |
1.92 |
2.32 |
1.18 |
|
T1* |
10.82 |
4.95 |
3.16 |
1.76 |
2.14 |
1.17 |
|
T2* |
12.47 |
6.71 |
3.04 |
0.75 |
0.83 |
0.19 |
| *Hours/24 | ||||||
|
SD_0 |
0.82 |
1.46 |
0.64 |
0.88 |
0.24 |
0.09 |
|
SD_1 |
1.21 |
1.43 |
0.34 |
0.77 |
0.27 |
0.16 |
|
SD_2 |
1.46 |
1.62 |
0.37 |
0.35 |
0.29 |
0.22 |
|
Table 2: mean hours of each behaviour in the three moments of the study (T) and standard deviation (SD) of each parameter |
||||||
RESULTS
Sleeping pattern
The results about sleeping (Table 3) show that OMT+SMT was effective in increasing rest hours in comparison with SMT alone (p=.005) and with no treatment (p=.001). However, there was no statistical significance between SMT and no treatment (p=.626). The normality test passed (p=0.066).
|
SLEEPING |
|||||
|
Comparison |
Diff of Means |
T |
Unadjusted P |
Critical Level |
Significant? |
|
T2vsT0 |
1.913 |
3.588 |
0.001 |
0.017 |
Yes |
|
T2vsT1 |
1.650 |
3.095 |
0.005 |
0.025 |
Yes |
|
T1vsT0 |
0.263 |
0.493 |
0.626 |
0.050 |
No |
|
Table 3: One way Analysis of Variance, Dependent Variable: Sleeping |
|||||
Awake & content pattern
The results on awake & content (Table 4) show that OMT+SMT was not significantly effective in increasing calm awake hours in comparison with SMT alone (p>.05). SMT had no significant effect in comparison and with no treatment (p>.05). While SMT+OMT was effective in increasing hours of awake and content in comparison with no treatment (p=.030). The normality test failed (p=.009)
AWAKE & CONTENT
|
Comparison |
Diff of Ranks |
q |
P<0.05 |
|
T2vsT0 |
99.000 |
3.556 |
Yes |
|
T2vsT1 |
78.000 |
2.802 |
No |
|
T1vsT0 |
21.000 |
0.754 |
No |
|
Table 4: One way Analysis of Variance on Ranks, Dependent Variable: Awake & content |
|||
Fussy pattern
The results about fussy (Table 5) show that OMT+SMT was effective in decreasing fussy hours in comparison with SMT alone (p<.001), while SMT showed no significant change in comparison with no treatment (p>.05). Moreover SMT+OMT was effective in decreasing fussy hours in comparison with no treatment (p<.001). The normality test failed (p=.000).
|
FUSSY |
|||
|
Comparison |
Diff of Ranks |
q |
P<0.05 |
|
T0vsT2 |
140.500 |
5.047 |
Yes |
|
T0vsT1 |
6.500 |
0.233 |
No |
|
T1vsT2 |
134.000 |
4.813 |
Yes |
|
Table 5: One way Analysis of Variance on Ranks, Dependent Variable: Fussy |
|||
Crying pattern
The results about crying (Table 6) show that OMT+SMT was effective in decreasing wept hours in comparison with SMT alone (p<.001), while SMT alone had no significant effects in comparison with no treatment (p>.05). Then SMT+OMT was effective in decreasing crying hours in comparison with no treatment (p<.001). The normality test failed (p=.001).
|
CRYING |
|||
|
Comparison |
Diff of Ranks |
q |
P<0.05 |
|
T0vsT2 |
178.000 |
6.394 |
Yes |
|
T0vsT1 |
56.000 |
2.012 |
No |
|
T1vsT2 |
122.000 |
4.382 |
Yes |
|
Table 6: One way Analysis of Variance on Ranks, Dependent Variable: Crying |
|||
Unsoothable crying pattern
The results on unsoothable crying (Table 7) show that OMT+SMT was effective in decreasing colic hours in comparison with SMT alone (p<.001), while SMT alone had no significant effects in comparison and with no treatment (p>.05). Furthermore SMT+OMT was effective in decreasing unsoothable crying hours in comparison with no treatment (p<.001). The normality test failed (p=.048).
|
UNSOOTHABLE CRYING |
|||
|
Comparison |
Diff of Ranks |
q |
P<0.05 |
|
T0vsT2 |
152.000 |
5.460 |
Yes |
|
T0vsT1 |
4.000 |
0.144 |
No |
|
T1vsT2 |
148.000 |
5.316 |
Yes |
|
Table 7: One way Analysis of Variance on Ranks, Dependent Variable: Unsoothable crying |
|||
Feeding pattern
The results on feeding are inconclusive, indeed the differences in the median values among the treatment groups are not great enough to exclude the possibility that the difference is due to random sampling variability. There is no statistically significant difference (p = 0.160).
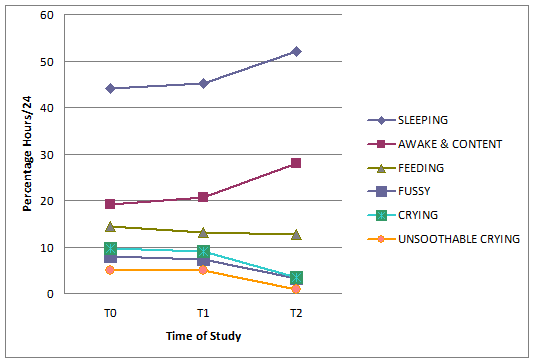
Meaning of results
In the 5 weeks of the study infants’ behaviour changed, with an increase in sleeping and awake and content trend, while a decrease in fussy, crying, unsoothable crying trend. Table 8 shows the mean time of hours/24 expressed in percentage at T0, T1, T2. Significant changes appear in unsoothable crying, which trend was about 5% hours/24 both at T0 and T1 was while less than 1% at T2. Similar results emerge from fussy behaviour which trend was more than 7% hours/24 both at T0 and T1 while about 3% at T2. Crying decreases from a trend that was about 9% hours/24 at T0 and T1, to a trend of about 3.5% at T2. Sleeping trend changes from about 44% at T0 to about 45% at T1, to about 52% at T2. Awake and content trend increases from about 19% at T0 to about 21% at T1, to about 28% at T2.
|
% |
SLEE- PING |
AWAKE & CON- TENT |
FEE- DING |
FUSSY |
CRYING |
UNSOOT-HABLE CRYING |
|
T0* |
43.99 |
19.10 |
14.34 |
7.99 |
9.65 |
4.93 |
|
T1* |
45.09 |
20.61 |
13.18 |
7.32 |
8.93 |
4.87 |
|
T2* |
51.96 |
27.98 |
12.65 |
3.14 |
3.47 |
0.80 |
| *% hours/24 | ||||||
|
Table 8: mean percentage of each parameter in the three moments of the study |
||||||
For each parameter there is a greater gap from T1 to T2 than T0 to T1 (graph 1).
Graph 1: percentage hours of each behaviour (sleeping, awake & content, feeding, fussy, crying, unsoothable crying) in the three moments of the study (T0, T1, T2)
DISCUSSION
Comparison of the outcomes
The results of the study show that OMT combined with SMT has an effect in babies with colic in a number of measurable variables.
In the current literature few studies about manipulative treatments on colic symptoms have been performed. Three systematic reviews [8,30-31] and a meta-analysis [9] have pointed out that there is little evidence about the effect of osteopathic treatment in colicky infants’ behaviour.
Nevertheless a UK pilot study has shown an improvement of colic symptoms after cranial osteopathic manipulation [13]. The differences between this and the current study are the variables analysed: the first considered only the parameters of crying and sleeping, while the current considered different types of crying (crying/unsoothable crying) and behaviour, such as fussy, feeding and calm awake. Because of the difference of the variables used, it is difficult to make comparisons between the results of the two studies, although both show significant improvement in the variables measured. The current research has aimed to widen the areas of treatment adding treatment that covers other body areas to the cranial manipulation. This method of evaluation of the entire body was used in a recent exploratory study on preterm infants with changes in gastrointestinal function: it has had positive results in reducing infants’ length of stay in hospital [33]. For this reason it was chosen this approach and not only cranial treatment.
Other studies using manipulative treatment on colicky babies have been done in the chiropractic field [10-12]. Also in these cases some systematic reviews declared the trials analysed small and prone to bias, so not able to give rigorous evidence [8-9,34-35].
However, different clinical trials have had encouraging results: since different medical interventions were studied but no therapy was shown to be completely effective [7-8,36], improvements with a non harmful treatment [40] can be object of interest in literature. Indeed some studies have shown great changes in infants’ behaviour after spinal manipulation both in the short [10,12] and the long term [37].
The variables evaluated were again not exactly the same as the current study, so it would be not correct compare these trials with the present. Moreover in these studies there is no explanation about the techniques used or the dysfunction treated, so it is not possible to compare between the chiropractic and osteopathic approaches.
Limitations of the study
The greatest limitation of the study is the small sample analysed. Although the power of the performed test was 0.886 with α=0.050, thus the sample appears adequate, a wider sample would have allowed to divide the group of treatment from the group of control. The small sample available was linked both to the very strict inclusion/exclusion criteria and the limited length of the enrolment period. The eligibility parameters were chosen on the basis of multiple studies that recognised various elements which may influence colic [8,16-18,38]. Excluding what can modify the phenomenon, there is less influence of other elements on the treatments adopted (OMT and SMT). But this narrowness excluded a lot of possible participants. But the availability of more recruitment time (in the current study it lasted 4 months) would have allowed a more robust project with adequate participants.
A further limitation of the current research is the length of the study (5 weeks) in comparison with the colic period (on average 12 weeks [1]). This aspect was related to the small sample again: clustering the groups of control and treatment the operator could involve double participants. With a wider sample a group could have received before SMT and then OMT and the other group the contrary. Or better each group could have received only one kind of treatment. It would be better because from a statistical point of view the maintenance of SMT during OMT creates not clear results (dragging effect). Moreover SMT may have needed more time to be effective, so it should be left at least the same time to act both for OMT and SMT to do an unbiased comparison (but the time of SMT was reduced to shorten the length of the study).
The choice of proposing both treatments was done for an ethical reason: OMT, is currently not recognised in Italy as a medical intervention, and therefore needed to be offered with a SMT.
To reduce the effect that the time has spontaneously on colic, infants were recruited as soon as possible. The mean age at the beginning of the study was 22.5 days therefore the study was completed when babies were less than 2 months old, age during which colic is normally present.
The last limit of the study was a difficult expressed by mothers to complete such rigorously and for so many days the diary. Although the diary used was validated [19,21,39], the variables analysed are based on people’s perception. It cannot be perfectly objective during a study, even more if people are no blind as in the current study.
Proposal for a larger study
The current research can be considered a pilot study for a next project that could have some different features: a wider sample and the separation of control and treatment groups.
To reduce the length of the study the frequency of OMT can be shortened, e.g. 1 treatment every 5 days. Indeed no adverse effect was recounted by parents and also in wider studies OMT was shown to have no contra-indications [40]. Keeping the preventive measures adopted (Appendix IV) it would be possible to bring the treatments closer to each other.
Eventually for the best clinical result OMT joined with a phytotherapic product may be added to other measures shown to have a role in relieving colic too [7-8,41].
CONCLUSION
The current study has shown that OMT combined with the use of a phytotherapic product appears to improve colic symptoms. In particular it has a role in reducing hours/24 spent in fussy, crying and unsoothable crying, moreover in increasing sleeping and awake & content time. A larger study is requested to make results more significant.
ACKNOWLEDGMENT
I would like to thank my supervisor Dr Patricia Burton for her support in projecting and completing the study and Dr Kerstin Rolfe for her precious advices about the statistical analysis.
I would like to thank Dr Alberto Maggiani who taught my what means doing research for his support in the first part of literature research.
I would like to thank all my teachers for their patient and passion in giving me their experience and for allowing me to end my studies in AIMO.
I would like to thank my parents without whom I would never have become an osteopath.
BIBLIOGRAPHIC REFERENCES
- Illingworth RS, (1954) Three months colic, Arch Dis Child; 29(145):165-74
- Reijneveld SA, Brugman E, Hirasing RA, (2001) Excessive infant crying: the impact of varying definitions, Pediatrics; 108(4):893-7
- Lucassen PL, Assendelft WJ, van Eijk JT, Gubbels JW, Douwes AC, van Geldrop WJ, (2001) Systemathic Review of occurrence of infantile colic in the community, Arch Dis Child; 84:398-403
- Roberts DM, Ostapchuk M, O’Brien JG, (2004) Infantile colic, Am Fam Physician; 70(4):735-40
- Illingworth R.S., (1985) Infantile colic revisited, Arch Dis Child: 60:981-985
- Miller-Loncar C, Bigsby R, High P, Wallach M, Lester B, (2004) Infant colic and feeding difficulties, Arch Dis Child; 89(10):908-12
- Joanna Briggs Institute, (2008) The effectiveness of interventions for infant colic, Aust Nurs J; 16(4):31-4
- Lucassen P, (2010) Colic in infants, Clin Evid; (Online)
- Dobson D, Lucassen PL, Miller JJ, Vlieger AM, Prescott P, Lewith G, (2012) Manipulative therapies for infantile colic, Cochrane Database Syst Rev; 12:CD004796
- Wiberg J.M.M, Nordsteen J, Nilsson N, (1999) The Short-term Effect of Spinal Manipulation in the Treatment of Infantile Colic: a Randomized Controlled Clinical Trial with a Blinded Observer, J Manipulative Physiol Ther; 22(8):517-22
- Olafsdottir E, Forshei S, Fluge G, Markestad T, (2001) Randomised controlled trial of infantile colic treated with chiropractic spinal manipulation, Arch Dis Child; 84(2):138-41
- Miller JE, Newell D, Bolton JE, (2012) Efficacy of chiropractic manual therapy on infant colic: a pragmatic single-blind, randomized controlled trial, J Manipulative Physiol Ther; 35(8):600-7
- Hayden C, Mullinger B, (2006) A preliminary assessment of the impact of cranial osteopathy for the relief of infantile colic, Complement Ther Clin Pract; 12(2):83-90
- Silver HK, Kempe CH, Bruyn HB, Fulginiti VA, (1987) Handbook of pediatrics, (eds Appleton & Lange). Norwalk: Conn
- Høgdall CK, Vestermark V, Birch M, Plenov G, Toftager-Larsen K, (1991) The significance of pregnancy, delivery and postpartum factors for the development of infantile colic, J Perinat Med; 19(4):251-7
- Wade S, Kilgour T, (2001) Extracts from “clinical evidence”: Infantile colic, BMJ; 323(7310):437-40
- Hill D.J, Roy N, Heine R.G, Hosking C.S, Francis D.E, Brown J, Speirs B, Sadowsky j, Carlin J.B, (2005) Effect of a low allergen maternal diet on colic among breastfeed infants: a randomised controlled trial, Pediatrics; 116(5):709-15
- Critch JN, Canadian Paediatric Society, Nutrition and Gastroenterology Committee, (2011) Infantile colic: Is there a role for dietary interventions?, Paediatr Child Health; 16(1):47-49
- St James-Roberts I, Conroy S, Wilsher K, (1996) Bases for maternal perceptions of infant crying and colic behaviour, Arch Dis Child; 75(5):375-84
- St James-Roberts I, Halil T, (1993) Infant crying patterns in the first year: normal community and clinical findings, J. Child Psychol psychiatry; 32(6):951-68
- Barr RG, Kramer M.S, Boisjoly C, McVey-White L, Pless I.B, (1988) Parental diary of infant cry and fuss behaviour, Arch Dis Child; 63(4):380-7
- St James-Roberts I, Goodwin J, Peter B, Adams D, Hunt S, (2003) Individual Differences in responsivity to a neurobehavioural examination predict crying patterns of 1-week-old infants at home, Dev Med Child Neurol; 45(6):400-7
- Magoun HI. (2008) Neonati e bambini. In: Osteopatia in ambito craniale, (eds. Futura Publishing Society) pp. 257-287
- Robbins KT, Fenton R.S, (1980) Jugular foramen Syndrome, J Otolaryngol; 9(6):505-16
- Pickar JG, (2002) Neurophysiological effects of spinal manipulation, Spine J; 2(5):357-371
- Lyubashina OA, Sokolov AY, Panteleev SS, (2012) Vagal afferent modulation of spinal trigeminal neuronal responses to dural electrical stimulation in rats, Neuroscience, [Epub ahead of print]
- da Silva RC, de Sà CC, Pascual-Vaca AO, de Souza Fontes LH, Herbella Fernandes FA, Dib RA, Blanco CR, Queiroz RA, Navarro-Rodriguez T, (2012) Increase of lower esophageal sphincter pressure after osteopathic intervention on the diaphragm in patients with gastroesophageal reflux, Dis Esophagus, [Epub ahead of print]
- Nelson KE, Glonek T, (2007) Somatic Dysfunction in Osteopathic Family Medicine. In: Procedures for treating conditions commonly encountered in family practice (Eds Lippincott Williams&Wilkins), pp. 253-254. Crawfordsville: R.R. Donnelley & Sons
- Gudmusson G, (2010) Infantile Colic: Is a pain Syndrome, Med Hypotheses; 75(6):528-529
- Cheung K, Hume P, Maxwell L, (2003) Delayed onset muscle soreness : treatment strategies and performance factors, Sports Med; 33(2):145-64
- Lucassen P, (2007) Infantile colic, Clin Evid (Online)
- Brand PL, Engelbert RH, Helders PJ, Offringa M, (2005) Systematic review of the effects of therapy in infants with the KISS-syndrome (kinetic imbalance due to suboccipital strain), Ned Tijdschr Geneeskd; 149(13):703-7
- Pizzolorusso G, Turi P, Barlafante G, Cerritelli F, Renzetti C, Cozzolino V, D’Orazio M, Fusilli P, Carinci F, D’Incecco C, (2011) Effect of osteopathic manipulative treatment on gastrointestinal function and length of stay of preterm infants: an exploratory study, Chiropr Man Therap; 19(1):15
- Ernst E, (2009) Chiropractic spinal manipulation for infant colic: a systematic review of randomised clinical trials, Int J Clin Pract; 63(9):1351-3
- Ernst E, Canter PH, (2006) A systematic review of systematic reviews of spinal manipulation, J R Soc Med; 99(4):192-6
- Garrison MM, Christakis DA, (2000) A systematic review of treatments for infant colic, Pediatrics; 106(1 Pt 2):184-90
- Miller JE, Phillips HL, (2009) Long-term effects of infant colic: a survey comparison of chiropractic treatment and nontreatment groups, J Manipulative Physiol Ther; 32(8):635-8
- Lucassen PL, Assendelft WJ, Gubbels JW, van Eijk JT, van Geldrop WJ, Neven AK, (1998) Effectiveness of treatments for infantile colic: systematic review, BMJ; 316(7144):1563-9
- St James-Roberts I, Hurry J, Bowyer J, (1993) Objective confirmation of crying durations in infants referred for excessive crying, Arch Dis Child; 68(1):82-4
- Colli R, Biagiotti I, Sterpa A, (2003) Osteopathy in neonatology, Pediatr Med Chir; 25(2):101-5
- Hunziker UA, Barr RG, (1986) Increased carrying reduces infant crying: a randomized controlled trial, Pediatrics; 7(5):641-8
Disegno di Legge 3270
Atti parlamentari Senato della Repubblica – N.3270
XVI LEGISLATURA – DISEGNI DI LEGGE E RELAZIONI – DOCUMENTI DISEGNO DI LEGGE
Art. 1.
(Oggetto e definizioni)
1. La presente legge, in attuazione dell’articolo 117, terzo comma, della Costituzione e nel rispetto dei princıpi dell’Unione europea in materia di concorrenza e di libertà di circolazione, disciplina le professioni non organizzate in ordini o collegi.
2. Ai fini della presente legge, per «professione non organizzata in ordini o collegi», di seguito denominata «professione», si intende l’attività economica, anche organizzata, volta alla prestazione di servizi o di opere a favore di terzi, esercitata abitualmente e prevalentemente mediante lavoro intellettuale, o comunque con il concorso di questo, con esclusione delle attività riservate per legge a soggetti iscritti in albi o elenchi ai sensi dell’articolo 2229 del codice civile, e delle attività e dei mestieri artigianali, commerciali e di pubblico esercizio disciplinati da specifiche normative.
3. L’esercizio della professione è libero e fondato sull’autonomia, sulle competenze e sull’indipendenza di giudizio intellettuale e tecnica, nel rispetto dei principi di buona fede, dell’affidamento del pubblico e della clientela, della correttezza, dell’ampliamento e della specializzazione dell’offerta dei servizi, della responsabilità del professionista.
4. La professione è esercitata in forma individuale, in forma associata, societaria, cooperativa o nella forma del lavoro dipendente. Nell’ipotesi di lavoro dipendente, i contratti di lavoro collettivi e individuali contengono apposite garanzie per assicurare l’autonomia e l’indipendenza di giudizio del professionista, nonchè l’assenza di conflitti di interessi, anche in caso di rapporto di lavoro a tempo parziale.
Art. 2.
(Associazioni professionali)
1. Coloro che esercitano la professione di cui all’articolo 1, comma 2, possono costituire associazioni a carattere professionale di natura privatistica, fondate su base volontaria, senza alcun vincolo di rappresentanza esclusiva, con il fine di valorizzare le competenze degli associati, diffondere tra essi il rispetto di regole deontologiche, agevolando la scelta e la tutela degli utenti nel rispetto delle regole sulla concorrenza.
2. Gli statuti e le clausole associative delle associazioni professionali garantiscono la trasparenza delle attività e degli assetti associativi, la dialettica democratica tra gli associati, l’osservanza dei principi deontologici, nonchè una struttura organizzativa e tecnico-scientifica adeguata all’effettivo raggiungimento delle finalità dell’associazione.
3. Le associazioni professionali promuovono, anche attraverso specifiche iniziative, la formazione permanente dei propri iscritti, adottano un codice di condotta ai sensi dell’articolo 27-bis del codice del consumo, di cui al decreto legislativo 6 settembre 2005, n. 206, vigilano sulla condotta professionale degli associati e stabiliscono le sanzioni disciplinari da irrogare agli associati per le violazioni del medesimo codice.
4. Le associazioni promuovono forme di garanzia a tutela dell’utente, tra cui l’attivazione di uno sportello di riferimento per il cittadino consumatore, presso il quale i committenti delle prestazioni professionali possano rivolgersi in caso di contenzioso con i singoli professionisti, ai sensi dell’articolo 27-ter del codice del consumo, di cui al decreto legislativo 6 settembre 2005, n. 206, nonchè ottenere informazioni relative all’attività professionale in generale e agli standard qualitativi da esse richiesti agli iscritti.
5. Alle associazioni sono vietati l’adozione e l’uso di denominazioni professionali relative a professioni organizzate in ordini o collegi.
6. Ai professionisti di cui all’articolo 1, comma 2, anche se iscritti alle associazioni di cui al presente articolo, non è consentito l’esercizio delle attivitàprofessionali riservate dalla legge a specifiche categorie di soggetti, salvo il caso in cui dimostrino il possesso dei requisiti previsti dalla legge e l’iscrizione al relativo albo professionale.
7. L’elenco delle associazioni professionali di cui al presente articolo e delle forme aggregative di cui all’articolo 3 che dichiarano, con assunzione di responsabilità dei rispettivi rappresentanti legali, di essere in possesso dei requisiti ivi previsti e di rispettare, per quanto applicabili, le prescrizioni di cui agli articoli 5, 6 e 7 è pubblicato dal Ministero dello sviluppo economico nel proprio sito internet, unitamente agli elementi concernenti le notizie comunicate al medesimo Ministero ai sensi dell’articolo 4, comma 1, della presente legge.
Art. 3.
(Forme aggregative delle associazioni)
1. Le associazioni professionali di cui all’articolo 2, mantenendo la propria autonomia, possono riunirsi in forme aggregative da esse costituite come associazioni di natura privatistica.
2. Le forme aggregative rappresentano le associazioni aderenti e agiscono in piena indipendenza e imparzialità.
3. Le forme aggregative hanno funzioni di promozione e qualificazione delle attività professionali che rappresentano, nonchè di divulgazione delle informazioni e delle conoscenze ad esse connesse e di rappresentanza delle istanze comuni nelle sedi politiche e istituzionali. Su mandato delle singole associazioni, esse possono controllare l’operato delle medesime associazioni, ai fini della verifica del rispetto e della congruità degli standard professionali e qualitativi dell’esercizio dell’attività e dei codici di condotta definiti dalle stesse associazioni.
Art. 4.
(Pubblicità delle associazioni professionali)
1. Le associazioni professionali di cui all’articolo 2 e le forme aggregative delle associazioni di cui all’articolo 3 pubblicano nel proprio sito web gli elementi informativi che presentano utilità per il consumatore, secondo criteri di trasparenza, correttezza, veridicità. Nei casi in cui autorizzano i propri associati ad utilizzare il riferimento all’iscrizione all’associazione quale marchio o attestato di qualità e di qualificazione professionale dei propri servizi, anche ai sensi degli articoli 7 e 8 della presente legge, osservano anche le prescrizioni di cui all’articolo 81 del decreto legislativo 26 marzo 2010, n. 59.
2. Il rappresentante legale dell’associazione professionale o della forma aggregativa garantisce la correttezza delle informazioni fornite nel sito web.
Art. 5.
(Contenuti degli elementi informativi)
1. Le associazioni professionali assicurano, per le finalità e con le modalità di cui all’articolo 4, comma 1, la piena conoscibilità dei seguenti elementi:
a) atto costitutivo e statuto;
b) precisa identificazione delle attività professionali cui l’associazione si riferisce;
c) composizione degli organismi deliberativi e titolari delle cariche sociali;
d) struttura organizzativa dell’associazione;
e) eventuali requisiti per la partecipazione all’associazione, con particolare riferimento ai titoli di studio relativi alle attività professionali oggetto dell’associazione, all’eventuale obbligo degli appartenenti di procedere all’aggiornamento professionale costante e alla predisposizione di strumenti idonei ad accertare l’effettivo assolvimento di tale obbligo e all’indicazione della quota da versarsi per il conseguimento degli scopi statutari;
f) assenza di scopo di lucro.
2. Nei casi di cui all’articolo 4, comma 1, secondo periodo, l’obbligo di garantire la conoscibilità è esteso ai seguenti elementi:
a) il codice di condotta con la previsione di sanzioni graduate in relazione alle violazioni poste in essere e l’organo preposto all’adozione dei provvedimenti disciplinari dotato della necessaria autonomia;
b) l’elenco degli iscritti, aggiornato annualmente;
c) le sedi dell’associazione sul territorio nazionale, in almeno tre regioni;
d) la presenza di una struttura tecnico-scientifica dedicata alla formazione permanente degli associati, in forma diretta o indiretta;
e) l’eventuale possesso di un sistema certificato di qualità dell’associazione conforme alla norma UNI EN ISO 9001 per il settore di competenza;
f) le garanzie attivate a tutela degli utenti, tra cui la presenza, i recapiti e le modalità di accesso allo sportello di cui all’articolo 2, comma 4.
Art. 6.
(Autoregolamentazione volontaria)
1. La presente legge promuove l’autoregolamentazione volontaria e la qualificazione dell’attività dei soggetti che esercitano le professioni di cui all’articolo 1, anche indipendentemente dall’adesione degli stessi ad una delle associazioni di cui all’articolo 2.
2. La qualificazione della prestazione professionale si basa sulla conformità della medesima a norme tecniche UNI ISO, UNI ENISO, UNI EN e UNI, di seguito denominate «normativa tecnica UNI», di cui alla direttiva 98/34/CE del Parlamento europeo e del Consiglio, del 22 giugno 1998, e sulla base delle linee guida CEN 14 del 2010.
3. I requisiti, le competenze, le modalità di esercizio dell’attività e le modalità di comunicazione verso l’utente individuate dalla normativa tecnica UNI costituiscono principi e criteri generali che disciplinano l’esercizio autoregolamentato della singola attività professionale e ne assicurano la qualificazione.
4. Il Ministero dello sviluppo economico promuove l’informazione nei confronti dei professionisti e degli utenti riguardo all’avvenuta adozione, da parte dei competenti organismi, di una norma tecnica UNI relativa alle attività professionali di cui all’articolo 1.
Art. 7.
(Sistema di attestazione)
1. Al fine di tutelare i consumatori e di garantire la trasparenza del mercato dei servizi professionali, le associazioni professionali possono rilasciare ai propri iscritti, previe le necessarie verifiche, sotto la responsabilità del proprio rappresentante legale, un’attestazione relativa:
a) alla regolare iscrizione del professionista all’associazione;
b) ai requisiti necessari alla partecipazione all’associazione stessa;
c) agli standard qualitativi e di qualificazione professionale che gli iscritti sono tenuti a rispettare nell’esercizio dell’attività professionale ai fini del mantenimento dell’iscrizione all’associazione;
d) alle garanzie fornite dall’associazione all’utente, tra cui l’attivazione dello sportello di cui all’articolo 2, comma 4;
e) all’eventuale possesso della polizza assicurativa per la responsabilità professionale stipulata dal professionista;
f) all’eventuale possesso da parte del professionista iscritto di una certificazione, rilasciata da un organismo accreditato, relativa alla conformità alla norma tecnica UNI.
2. Le attestazioni di cui al comma 1 non rappresentano requisito necessario per l’esercizio dell’attività professionale.
Art. 8.
(Validità dell’attestazione)
1. L’attestazione di cui all’articolo 7, comma 1, ha validità pari al periodo per il quale il professionista risulta iscritto all’associazione professionale che la rilascia ed è rinnovata ad ogni rinnovo dell’iscrizione stessa per un corrispondente periodo. La scadenza dell’attestazione è specificata nell’attestazione stessa.
2. Il professionista iscritto all’associazione professionale e che ne utilizza l’attestazione ha l’obbligo di informare l’utenza del proprio numero di iscrizione all’associazione.
Art. 9.
(Certificazione di conformità a norme tecniche UNI)
1. Le associazioni professionali di cui all’articolo 2 e le forme aggregative di cui all’articolo 3 collaborano all’elaborazione della normativa tecnica UNI relativa alle singole attività professionali, attraverso la partecipazione ai lavori degli specifici organi tecnici o inviando all’ente di normazione i propri contributi nella fase dell’inchiesta pubblica, al fine di garantire la massima consensualità, democraticità e trasparenza. Le medesime associazioni possono promuovere la costituzione di organismi di certificazione della conformità per i settori di competenza, nel rispetto dei requisiti di indipendenza, imparzialità e professionalità previsti per tali organismi dalla normativa vigente e garantiti dall’accreditamento di cui al comma 2.
2. Gli organismi di certificazione accreditati dall’organismo unico nazionale di accreditamento ai sensi del regolamento (CE) n. 765/2008 del Parlamento europeo e del Consiglio, del 9 luglio 2008, possono rilasciare, su richiesta del singolo professionista anche non iscritto ad alcuna associazione, il certificato di conformità alla norma tecnica UNI definita per la singola professione.
Art. 10.
(Vigilanza e sanzioni)
1. Il Ministero dello sviluppo economico svolge compiti di vigilanza sulla corretta attuazione delle disposizioni della presente legge.
2. La pubblicazione di informazioni non veritiere nel sito web dell’associazione o il rilascio dell’attestazione di cui all’articolo 7, comma 1, contenente informazioni non veritiere, sono sanzionabili ai sensi dell’articolo 27 del codice del consumo, di cui al decreto legislativo 6 settembre 2005, n. 206, e successive modificazioni.
Art. 11.
(Clausola di neutralità finanziaria)
1. Dall’attuazione degli articoli 2, comma 7, 6, comma 4, e 10 non devono derivare nuovi o maggiori oneri a carico del bilancio dello Stato. Il Ministero dello sviluppo economico provvede agli adempimenti ivi previsti con le risorse umane, strumentali e finanziarie disponibili a legislazione vigenti.
Artrosi
L’artrosi è una patologia degenerativa delle strutture articolari (nello specifico una perdita di cartilagine) che comunemente si verifica in articolazioni che per molto tempo sono state sollecitate, soprattutto quelle di maggior carico: anca, ginocchio, vertebre lombari. Il sintomo classico dell’artrosi è dolore mattutino a livello dell’articolazione interessata, che si allevia dopo i primi movimenti. Al dolore si associa un’importante rigidità articolare, che aumenta con la progressione dello stato degenerativo. Il trattamento osteopatico, che non può impedire questo processo molto comune nell’anziano, può tuttavia accompagnarlo rallentando la perdita di funzionalità delle articolazioni coinvolte e riducendo il dolore. Il trattamento consiste in tecniche specifiche di trazione e mobilizzazione per il recupero della funzionalità articolare e l’inibizione della muscolatura circostante l’articolazione stessa. Con un lavoro specifico, associato a un’adeguata e mirata attività fisica leggera, è possibile ritardare la necessità di una protesi. L’intervento osteopatico è inoltre di fondamentale importanza per evitare il sovraccarico di altre regioni del corpo che vengono eccessivamente utilizzate come compenso alla zona ipomobile e dolente.
Dolore lombare e cervicale
Tali disturbi colpiscono spesso le persone già dall’età adulta, con maggiore frequenza in chi ha precedentemente subito colpi di frusta, traumi di vario tipo o blocchi acuti. Il dolore può essere causato dalla componente muscolare, che si trova in uno stato tensivo alterato, e/o dalle articolazioni vertebrali rigide o artrosiche. Il dolore a livello cervicale può risultare molto fastidioso per le normali attività quotidiane (cucire, stirare, leggere) e diventare debilitante quando si evolve anche in cefalea. Il dolore lombare può addirittura impedire attività fisiche come camminare, andare in bicicletta, fare le scale. Consapevoli del fatto che essere limitati nei movimenti quotidiani riduce di molto la qualità di vita di un anziano, ci adoperiamo perchè questi disturbi rimangano silenti il più a lungo possibile. L’osteopatia infatti non può impedire i normali processi degenerativi e di alterazione a carico dei tessuti sulla base delle variazioni metaboliche che avvengono nell’anziano. L’osteopata può però ridurre questi sintomi lavorando sulle strutture interessate attraverso l’inibizione della muscolatura coinvolta, il recupero della mobilità e del drenaggio articolare, con tecniche dolci e delicate, per nulla invasive. Può quindi evitare o ridurre la necessità di una terapia antidolorifica che in un anziano può affaticare il fegato, generalmente già sotto stress per l’utilizzo di altri farmaci.
Rigidità articolare e difficoltà al movimento
Con il tempo nelle articolazioni, in particolare in quelle sottoposte a maggior carico (anca, ginocchio, vertebre lombari), vengono a ridursi lo spessore cartilagineo, il drenaggio e la lubrificazione. Questo fa parte di un fisiologico processo che vede modificarsi le varie attività metaboliche, dal momento in cui termina lo sviluppo in poi. La principale conseguenza è una maggior rigidità articolare che provoca impaccio e difficoltà al movimento, specialmente nelle persone che conducono una vita sedentaria. Il trattamento osteopatico non può impedire il processo degenerativo a carico dei tessuti, ma può accompagnarlo rallentandone la progressione, attraverso tecniche dolci che vanno ad aumentare la mobilità delle articolazioni, che ne migliorano il drenaggio e che favoriscono una riduzione dello stato tensivo dei muscoli circostanti le articolazioni stesse. Una migliore funzionalità articolare permette movimenti più liberi e sciolti, quindi minor impaccio nelle attività quotidiane e un ridotto rischio di cadute e traumi. Maggior libertà di movimento significa anche la possibilità di praticare attività fisica, dalla passeggiata quotidiana alla ginnastica dolce, il che è fondamentale per un mantenimento ottimale dei risultati ottenuti con il trattamento manipolativo.
Rigidità e blocchi articolari
La rigidità articolare può essere un ostacolo a una performance fisica ottimale. Può comparire nello sportivo a causa di un’eccessiva sollecitazione di determinate articolazioni con lo sforzo fisico o traumi. Ancora può essere dovuta posizioni scorrette mantenute durante l’attività sportiva o lavorativa. In caso di episodio acuto, solitamente a seguito di un movimento brusco e traumatico o per microtraumi ripetuti, la rigidità si può trasformare in blocco articolare. L’osteopata interviene individuando le disfunzioni articolari e correggendole attraverso una manipolazione mirata. Il trattamento osteopatico si prefigge inoltre di prevenire ulteriori blocchi approcciando il resto della colonna vertebrale in modo che lavori in modo più armonioso. Spesso una rigidità cronica si accompagna anche a una contrattura della muscolatura paravertebrale. In questo caso il trattamento comprende, oltre alle tecniche articolatorie e manipolative, anche l’inibizione specifica della muscolatura coinvolta.