Di Francesco Badi
Abstract
Urinary incontinence caused by Detrusor Overactivity is a common problem between men suffering from Parkinson’s disease caused by the neurological degeneration of the dopaminergic neurones and this kind of symptoms could have an effect on Quality of Life of these patients. In particular nocturia and urinary urgency are the most annoying symptoms complained by patients. The aim of the present study was to evaluate whether osteopathic treatment could improve the urinary symptoms severity and have an effect on the Quality of Life.
MATERIALS AND METHODS: From 40 potential patient, 10 have been enrolled in the protocol, divided in two groups and the OAB-questionnaire was submitted to see changes before and after treatments. The patient of the Group 1 was treated before with 3 real osteopathic treatments and after with 3 “sham” treatments. The patient of the Group 2 did the opposite. OAB-q data were statistical analysed and compared.
STATISTICAL ANALYSIS: ANOVA: Data were analysed comparing data before treatments, after real osteopathic treatments, after sham treatments. ANOVA analysis of variance were used to analyse the variables that passed normality test except for “social” that was analysed with a Kruskal Wallis test. P was set at <0.05.
RESULTS: The results show no statistical significance for any variable but analysing the trend of the means of the single variable there are changes in every variable except for “sleep”.
CONCLUSION: Osteopathy seems not to be helpful in improving the quality of life of patient with incontinence suffering from Parkinson’s disease but it is worth to propose a larger study with a bigger sample of patient to clear these results.
INTRODUCTION
Parkinson’s disease (PD) is a neurological degenerative affection caused by the progressive loss of the dopaminergic neurones of the pars compacta in the substantia nigra of the basal ganglia. It affects 13.4 per 100,000 of the population (1). The typical clinical findings in these patients are: tremor, rigidity and bradikynesia (2). In addition to these symptoms there are also other non-motor symptoms in which there are depression, anxiety, sleep disorders, cognitive disorders (3) and autonomic disorders that can cause bladder dysfunction and urinary incontinence. The incidence of Lower Urinary Tract (LUT) disease has been estimated between 55% and 80% of PD patients (4). In Parkinson’s patients the thought is that the neural degeneration is not limited to basal ganglia but it involves other neural transmission systems outside the brain and the spinal cord (2). The voiding function is controlled by the pontine micturition centre (PMC) and it has been shown that it is facilitated by the hypothalamus, cerebellum, basal ganglia and frontal cortex (5). Studies suggest that bladder voiding is under the inhibitory control of the basal ganglia (5,6,7). These ganglia can control the dopaminergic neurons in the striatus nucleus which is responsible for the inhibition of the micturition reflex with a GABA-ergic circuit (8).
Sometimes the clinical findings about incontinence are not so clear because, in addition to a neurological problem due to the PD, other obstructive syndromes such as bladder outlet obstruction can be reported and this makes the diagnosis more complex (9). It has been found correlation between bladder dysfunction and neurological disorders in patients suffering from Parkinson’s disease (10) and between bladder dysfunction and stage of the disease (11). Another study by Campos-Sousa et al. did not find a correlation between the neurological degeneration and LUT symptoms (12). Of the symptoms complained of nocturia is the most common among Parkinon’s patients (>60%) (10,11,12). Detrusor overactivity has been found in 45-93% (13) and a relaxation of the external sphincter in 33% of the cases (14).
In literature there are no articles about manual treatments in this kind of patient but there are some authors that underline the importance of the treatment of the pubo-prostatic ligaments to improve the continence in overactive bladder (15,16). Studies mention some parts of the body that if treated may help to balance the autonomic nervous system and reduce stress on the walls of the bladder so as to improve the continence(17).
Study Aims
The aim of this study was to investigate whether osteopathic treatment has an effect on:
1. Urinary incontinence in men suffering of PD
2. The Quality of Life of men suffering of PD.
The hypothesis was that the treatment of the Dorsal-Lumbar spine, which is the tract of the sympathetic innervation of the LUT, and the treatment of the pelvic floor and thoracic diaphragm, to balance the intra-abdominal pressure, could improve the voiding symptoms in these patients and affect their Quality of Life.
METHODOLOGY
Participants
Participants were men recruited from the degenerative illness division of the Valduce Hospital in Como, Italy who were invited to participate in the study. From 40 men between 50 to 70 years old identified as potential patients, 10 men decided to join the study. To enter the study they must have suffered from Parkinson’s Disease for over 5 years and from urinary incontinence for over 2 years. Patients who have had tumours or surgical intervention on the bladder were excluded from the study, also excluded was a patient who had a LUT infection during the clinical trial. Patients also suffering from other disease e.g. Diabetes Mellitus were excluded. (Table 1)
| INCLUSION | EXCLUSION | |
| AGE | 50-70 years old | <50years >70years |
| PARKINSON | >5 years | <5 years |
| INCONTINENCE | >2 years | <2 years |
| SURGICAL INTERVENTION ON BLADDER | No | Yes |
| LUT INFECTION | No | Yes |
| OTHER DISEASE | No | Yes |
Table 1: Inclusion/Exclusion criteria.
Materials & Methods
Men were selected among the degenerative illness division of the Valduce hospital and evaluated by Dr Corengia who assessed the risk and benefits of the osteopathic treatment and who determined whether the patients were appropriate to be included in the study.
An information sheet about the study explaining the aims, the procedure, the single treatment (Appendix I) and Risk Assessment Sheets (Appendix II) was given to the subjects. Participants were also required to sign a consent form after joining the study (Appendix III). The validated Overactive Bladder Questionnaire (18,19) was given to participants to assess the initial urinary symptoms and Quality of Life rating and to monitoring the improvements with OMT before and after treatments (3,20) (Appendix IV).
Experimental Procedure
The 10 patients who were recruited to take part to the study were randomly divided in two groups:
Group 1_ Subjects were treated with OMT for three times and after with a sham treatment for another three times with a wash out period of two weeks between OMT and sham
Group 2_ Subjects were treated with sham treatment before for three times, and after with OMT for another three times with a wash out period of two weeks between sham and OMT.
Osteopathic Treatment: Subjects were treated with mobilization of the dorsal-lumbar spine because of the sympathetic innervation of the LUT trying to balance the sympathetic autonomic system, and had the thoracic diaphragm and pelvic diaphragm assessed because of the intra-abdominal pressure that can cause incontinence. Patients had their pubic symphysis and the pubo-prostatic ligament of the urogenital diaphragm assessed with palpation because the fascial treatment of these ligaments improve the bladder continence (15,16,17).
Sham treatment: Subjects were treated at a different part of the body so as not to interfere with the intervention treatment. The sham treatment was designed to appear as a valid treatment to the subjects.
Subjects were sham treated on the Lower Limb so as not to interfere with the interventional treatment. The sham treatment had interventional parameters equal to the treatment but on the “neutral “ area.
Apparatus
The OAB-questionnaire was given to participants before any treatments started, after real osteopathic treatments and after the sham treatments. The Overactive Bladder Questionnaire (OAB-q) is a multidimensional instrument designed to assess patient perception of symptom complained and its impact on health-related quality of life (HRQL) among patients with Overactive Bladder. This questionnaire is composed of 33 items that involves the evaluation of the urinary symptoms severity and its affect on the Quality of Life in the first 8 items, and the other 25 items are a general investigation of the Quality of Life of the subjects through the evaluation of different aspects (concern, coping sleep, social interaction) (18).
Ethical Issues
The subjects were recruited by invitation to voluntarily take part in the study. All questionnaires were anonymous. The subjects retained the right to stop the procedure and leave the study at any point, without giving a reason. Their ongoing drug treatment was neither stopped nor changed during the research project. The ethic form was submitted and approved by BCOM (Appendix V).
STATISTICAL ANALYSIS
Data were analysed comparing data before treatments, after real osteopathic treatments, after sham treatments. A normality test was run (Shapiro Wilk) for this data. Every variable passed the normality test except for the “social” variable. ANOVA was used on the variables that passed normality, the “social” variable (that failed normality)was analysed with a Kruskal Wallis test. The means of the single variable were also analysed to see changes even without a statistical significance. P was set at <0.05.
RESULTS
All of the 10 patient complete the study no one quitted it. The mean age of the participants was 67.5 years old.
The results show no statistical significance with the ANOVA analysis. No differences has been found with the variable “group”.
“Symptoms Severity”, though the symptom results show a trend of improvement for both post OMT and post sham this did not reach statistical significance (F=0.529 p=0.595; Graph 1). Sleep showed no change over the three interventions (F=0.086; p=0.018; Graph 2)
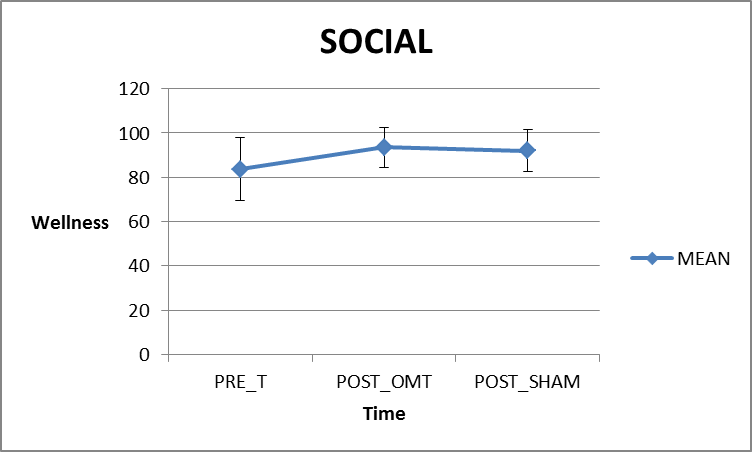
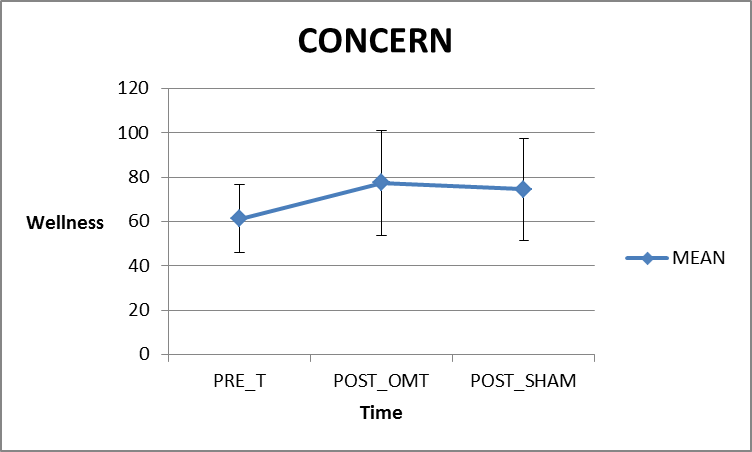
“Coping’ showed no significant difference between pre, post OMT or post Sham (F=0.421 p=0.661; Graph 4). ‘Social’ showed a slight improvement from the pre questionnaire but did not reach statistical significance (Kruskal Wallis test, H=3.614, p=0.164; Graph 3). ‘Concern’ though the symptom results show a trend of improvement for both post OMT and post sham this did not reach statistical significance (F=1.661, p=0.209; Graph 5).
 GRAPH 1: Symptom severity (0=no symptoms). Graph showing the mean values of the Overactive Bladder Questionnaire. Error bars= SD and n=10. There was no statistical significance for any group. There is a slight improvement from pre-treatments and after OMT treatments but after the sham treatments there is a little worsening. A global improvement from before treatments and after treatments.
GRAPH 1: Symptom severity (0=no symptoms). Graph showing the mean values of the Overactive Bladder Questionnaire. Error bars= SD and n=10. There was no statistical significance for any group. There is a slight improvement from pre-treatments and after OMT treatments but after the sham treatments there is a little worsening. A global improvement from before treatments and after treatments.
GRAPH 2: Sleep (100 =complete wellbeing ). Graph showing the mean values of the Overactive Bladder Questionnaire. Error bars= SD and n=10. There was no statistical significance for any group. There is no substantial changes between before and after treatments.
GRAPH 3: Social (100 =complete wellbeing ). Graph showing the mean values of the Overactive Bladder Questionnaire. Error bars= SD and n=10. There was no statistical significance for any group. There is a slight improvement between pre- treatments and after OMT treatments and a little worsening after the sham treatments. A global improvement from the beginning of the therapy to the end.
GRAPH 4: Coping (100 =complete wellbeing ). Graph showing the mean values of the Overactive Bladder Questionnaire. Error bars= SD and n=10. There was no statistical significance for any group. There are no substantial changes between before treatments and after OMT, and a slight improvement after the sham treatments.
GRAPH 5: Concern (100=complete wellbeing ). Graph showing the mean values of the Overactive Bladder Questionnaire. Error bars= SD and n=10. There was no statistical significance for any group. There is an improvement from before treatments and after OMT treatments, and a little worsening after the sham treatments.
DISCUSSION
Urinary incontinence caused by neurogenic Detrusor Overactivity is a common finding in patients suffering from Parkinson’s disease, and its affect the quality of life, emotional well-being and productivity at work (21).
The OAB-questionnaire is a validated questionnaire to identify Overactive Bladder (OAB) that a symptom-based condition defined as “urinary urgency with or without incontinence, often with increased urinary frequency and nocturia” (18,19). Although the results from this current study did not reach a statistical significance, the means of the single variables suggest that there are a trends of improvements in the variables “symptoms severity” “social” and “concern” after OMT treatments and no substantial changes in the variable “sleep”, which did not have changes, and “coping” which has a slight improvement after the sham treatments. In a general overview of the means of the single variable which are not statistically significant, it can be noticed that between before and after all treatments there is an improvement in every variable except for “sleep”. In the current literature there are no other studies about manual treatments and Overactive Bladder. The small number of patients led to slight results in symptoms severity with no statistical significance, but the mean differences suggest that Osteopathic Manual Treatment could have an effect of these symptoms and on the Quality of Life of the patients.
Detrusor Overactivity is thought to be the most probable cause of Overactive Bladder (22) but there is also another condition that can cause similar urinary symptoms: the Bladder Outlet Obstruction (e.g. prostatic hypertrophy). The Bladder Outlet Obstruction is a common condition that can affect men over 50 years old and can be added to a clinical condition of Overactive Bladder (23). For these reasons it cannot be reported if the Osteopathic treatment had an effect during this intervention on autonomic nervous system balancing the sympathetic and parasympathetic system or intervention reducing mechanical stress over the bladder and Lower Urinary Tract. Furthermore the Bladder Outlet Obstruction can change the afferent nervous signal from the Lower Urinary Tract itself and cause an imbalance of the sympathetic/parasympathetic system (24).
The Quality of Life of these patients is heavily affected by the urological symptoms that can reduce the sleeping time, social interaction and increase the time spent at home (25).
It is well known that osteopathy can significantly affect the Quality of Life of patients with several pathologies (26,27) however this current study did not show any significant changes in the quality of like of these patients. This may be due to the limitations discussed later in this paper.
Limits of the study
The small sample of patients is a great limitation of the current study, the statistical tests showed that each variable was under powered (<0.8) and a sample size calculation suggested a minimum of 50 participants would be needed. The inclusion/exclusion criteria limited the size of the sample because women and men have anatomical differences and different types of incontinence caused by other reasons; for these reasons the sample was exclusively men (28). Furthermore we have no difference between pre-treatments and post-treatments statistically significant so we cannot consider these results as positive results. This could be due to the small sample of patient that is hard to find among Parkinson’s patient because is a problem underrated by doctors and the patients are not stimulate to complain about these symptoms because they feel embarrassed. It could have been used a more specific questionnaire on bladder symptoms perception in addition to OAB-q such as the PPBC (Patient Perception Bladder Condition) (29). The study would have been more specific with the help of objective measures for instance a cystometry or urodynamic exams to assess the initial level of the disease and the changes after treatments (30). The short time of recruitment may be considered as a limitation because patients with these characteristics are available only in particular clinics or hospitals and they have only a small number of patients.
CONCLUSION
The current study show that osteopathy cannot change aspects of the Quality of Life in patient suffering from incontinence and Parkinson’s disease. Some changes were recorded with the trend of the analysis of the means so further studies with a larger sample of patients are needed to clear these aspects.
References:
- Stephen K. Van Den Eeden, Caroline M. Tanner, Allan L. Bernstein, Robin D. Fross, Amethyst Leimpeter1 Daniel A. Bloch, and Lorene M. Nelson, Incidence of Parkinson’s Disease: Variation by Age, Gender, and Race/Ethnicity, American Journal of Epidemiology,2003 Vol. 157, No. 11.
- Sakakibara R, Tateno F, Kishi M, Tsuyuzaki Y, Uchiyama T, Yamamoto T., “Pathophysiology of bladder dysfunction in Parkinson’s disease.” Neurobiological Disease. 2012 Jun;46(3):565-71.
- Kristine K. Hanna and Alice Cronin-Golomb “Impact of Anxiety on Quality of Life in Parkinson’s Disease” Parkinson’s Disease 2012, Article ID 640707
- McGrother, C.W., Jagger, C., Clarke, M., Castleden, C.M., 1990. Handicaps associated with incontinence: implications for management. Journal of Epidemiology and Community Health 44,246–248.
- Kavia, R.B.C., Dasgupta, R., Fowler, C.J., 2005. Functional imaging and the central control of the bladder. Journal of Comparative Neurology 493, 27–32.
- De Groat, W.C., 2006. Integrative control of the lower urinary tract: preclinical perspective.British Journal of Pharmacology 147, S25–S40.
- Blackett H, Richard Walker, Brian Wood, “Urinary dysfunction in Parkinson’s disease: A review” Parkinsonism and Related Disorders 15 (2009) 81e87
- Dalmose, A.L., Bjarkam, C.R., Sorensen, J.C., Djurhuus, J.C., Jorgensen, T.M., 2004. Effects of high frequency deep brain stimulation on urine storage and voiding function in conscious minipigs. Neurourology and Urodynamics 23, 265–272.
- Gina A Defreitas, Gary E Lemack, Philippe E Zimmern, Richard B Dewey, Claus G Roehrborn, Padraig E O’Suilleabhain, “Distinguishing neurogenic from non-neurogenic detrusor overactivity: a urodynamic assessment of lower urinary tract symptoms in patients with and without Parkinson’s disease” Urology. 2003 Oct;62(4):651-5.
- Araki I, Kitahara M, Oida T, Kuno S. “Voiding dysfunction and Parkinson’s disease: urodynamic abnormalities and urinary symptoms”. Journal of Urology 2000 Nov;164(5):1640-3.
- Sakakibara, R., Shinotoh, H., Uchiyama, T., Sakuma, M., Kashiwado, M., Yoshiyama, M., Hattori, T., 2001. Questionnaire-based assessment of pelvic organ dysfunction in Parkinson’s disease. Autonomic Neuroscience:Basic&Clinical. 92, 76–85.
- Campos-Sousa, R.N., Quagliato, E., da Silva, B.B., De Jr., C.R., Ribeiro, S.C., de Carvalho, D.F., 2003. Urinary symptoms in Parkinson’s disease: prevalence and associated factors. Arquivos de Neuropsiquiatria 61, 359–363.
- Palleschi G, Pastore AL, Stocchi F, Bova G, Inghilleri M, Sigala S, Carbone A., “Correlation between the Overactive Bladder questionnaire (OAB-q) and urodynamic data of Parkinson disease patients affected by neurogenic detrusor overactivity during antimuscarinic treatment.” Clin Neuropharmacol. 2006 Jul-Aug;29(4):220-9.
- Hattori, T., Yasuda, K., Kita, K., Hirayama, K., 1992. Voiding dysfunction in Parkinson’s disease. Jpn. J. Psychiatry Neurol. 46, 181–186
- Raymond E PooreA, David L McCulloughA, Jonathan P JarowA, Puboprostatic Ligament Sparing Improves Urinary Continence After Radical Retropubic Prostatectomy,Urology, Volume 51, Issue 1, January 1998, Pages 67–72
- Siamak Daneshmand, David A. Ginsberg, James K. Bennet, Jenelle Foote, Wylly Killorin, Kevin P. Rozas, Bruce G. Green, Puboprostatic Sling Repair for Treatment of Urethral Incompetence in Adult Neurogenic incontinence, Journal of Urology, Volume 169, Issue 1, January 2003,
- Kuchera M. Kuchera W “Osteopathic consideration in systemic disfunction” Columbus Greyden Press 1994, Osteopathic consideration in genitourinary tract disorders;
- Coyne KS, Matza LS, Thompson CL. The responsiveness of the Overactive Bladder Questionnaire (OAB-q). Quality of Life Research 2005;14(3): 849Y855.
- Wein AJ. Diagnosis and treatment of the overactive bladder. Urology. 2003 Nov;62(5 Suppl 2):20-7.
- Karin S. Coyne, Chris C. Sexton, Debra E. Irwin*, Zoe S. Kopp†, Con J. Kelleher‡ and Ian Milsom The impact of overactive bladder, incontinence and other lower urinary tract symptoms on quality of life, work productivity, sexuality and emotional well-being in men and women: results from the EPIC study, BJU International Journal (2008)| 101 , 1 3 8 8 – 1 3 9 5
- Debra E Irwin, Ian Milsom, Zoe Kopp, Paul Abrams, Linda Cardozo, Impact of overactive bladder symptoms on employment, social interactions and emotional well-being in six European countries, BJU International volume 97, Issue 1, pages 96–100, January 2006
- Andersson KE. The overactive bladder: pharmacologic basis of drug treatment . Urology 1997 ; 50 ( 6A Suppl ): 74 – 84
- Ali A, Al-Zahrani AA, Gajewski JB. Association of symptoms with urodynamic findings in men with overactive bladder syndrome. BJU International 2012 Dec;110(11 Pt C):E891-5.
- Dobrek L, Baranowska A, Skowron B, Thor PJ. Autonomic nervous system activity assessement by heart rate variability in experimental bladder outlet obstruction Postepy Hig Med Dosw (Online). 2013 Apr 2;67(0):221-8.
- Espuña-Pons M, Castro-Díaz D, Díaz-Cuervo H, Pérez M. Impact of overactive bladder treatment on the quality of life of patients over 60 with associated pathologies Archivos Espanoles de Urologia. 2013 Apr;66(3):287-294.
- Florance BM, Frin G, Dainese R, Nébot-Vivinus MH, Marine Barjoan E, Marjoux S, Laurens JP, Payrouse JL, Hébuterne X, Piche T Osteopathy improves the severity of irritable bowel syndrome: a pilot randomized sham-controlled study, European Journal of Gastroenterology and Hepatology. 2012 Aug;24(8):944-9
- Papa L, Mandara A, Bottali M, Gulisano V, Orfei S. A randomized control trial on the effectiveness of osteopathic manipulative treatment in reducing pain and improving the quality of life in elderly patients affected by osteoporosis. Clin Cases Miner Bone Metab. 2012 Sep;9(3):179-83.
- Giarenis I, Mastoroudes H, Srikrishna S, Robinson D, Cardozo L. Is there a difference between women with or without detrusor overactivity complaining of symptoms of overactive bladder? BJU International 2013 Mar 4.
- Karin S. Coyne a, Louis S. Matzaa, Zoe Koppb, Paul Abrams, The Validation of the Patient Perception of Bladder Condition (PPBC): A Single-Item Global Measure for Patients with Overactive Bladder, European Urology 49 (2006) 1079–1086
- Simn Jackson, The patient with an overactive bladder—Symptoms and quality-of-life issues, Urology volume 50, Issue 6, Supplement 1, December 1997